This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome.
This is a case of a 33 year old male patient auto driver by occupation who came to hospital with the chief complaints of pus discharge from his left upper molar teeth into his mouth since 2 months.
Patient history:
At the age of 1 year he had trauma to his left eye by a sharp object then his parents took him to an ophthalmologist, and surgery couldn't be done due to their financial issues.
Now he has only his right eye having vision of 6/6 and left eye completely lost it's vision.
He studied till grade 10 dropped out from the school and then in the year 2005 at the age of 16 he came to Bangalore in search of work and started working as a construction worker. He further visited several hospitals for his vision, where surgery was recommended which he wasn't willing to have.
He also says that he had periodic cough and cold episodes more during winters lasting for more than a week occasionally and releived on medications.
There due to peer pressure he started having alcohol nearly once a week 40-50ml per day. He also started smoking around the same time 1-2 cigarettes per day which increased to 3-4/day over years. He stopped his alcohol consumption and smoking since 10 years. He also has a habit of tobacco chewing 3 times a day since 5 years which he retains under his lip for nearly 15 mins.
He occasionally used to visit his home every 3-6 months.
In the year 2013 he went to his home place, got married and settled down there and started farming. He farms potatoes rice and chillies.
In the year 2015 he started business with his friend who was also his business partner, as things didn't go so well they got into a fight where he complains of injury to his upper jaw which was not so severe and resolved soon.
In the year 2016 he started working as an auto driver. He gets up daily at around 7 AM, has his breakfast and leaves to works at around 8 30 AM comes back at 7 30 PM in the evening and sleeps at 11pm.
He says that during childhood lost teeth didn't fully grow in number and he had only 14 tooth in his upper jaw and 16 in the lower. And he had empty space left in that area.
In the year 2021 December, i.e, 2 months ago he noticed a swelling in the gaps which was painful. He assumed that tooth is arising from that area. He then used some painkillers and pain was releived. 3 days later, pus was oozing out as the swelling was cut while he was consuming fish. Over 9 days pain was gradually progressive. He then approached a local doctor, took medications, it releived.
4 days later it burst and yellowish white foul smelling, mucoid, pus was oozing out profusely between his left second and third upper molar teeth which was coming into his mouth. It was continuous, occasionally blood stained associated with swelling over the left cheek and pain which was continuous, throbbing type . It aggravated on pinching his nostrils and creating pressure inside his mouth, movement of jaw and stretching his mouth. He initially got a discharge of nearly 50 ml per day for a few days.
No h/o ear nose and throat symptoms, headache, swelling, pain over the sinuses, redness .
He presses his nose with mouth closed and create pressure inside the mouth so that pus comes out and he spits it out . Then for an hour or so discharge stops. Meanwhile he takes his food. An hour later it appears again.
On 4 Jan 2021, he approached a dentist, where he was given medications which he used them for 3 days and there was no relief.
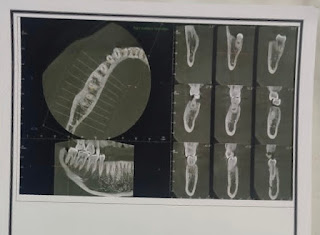
He was told to have his OPG and CBCT scan done on the same day, where he was told he needs and surgery and was told to refer OMFS department.
He was given Tab. augmentin, Voveran tab., Metrogyl tab.
On 22/1/22 he got his OPG and CBCT reports after which he was given tab. taxim which he didn't use.
CBCT scan reports-
OPG report-
Radiological diagnosis-
On 5/2/22 he noticed blood discharging from the same area following which he took tab. cefotaxim on which his pain releived. His pain almost subsided by the time he came here to the hospital.
Past history-
No h/o similar complaints in the past
No h/o diabetes, hypertension, tb, asthma, epilepsy
No h/o dental extractions.
No h/o dental surgeries
Personal history-
Diet- mixed
Appetite- good
Sleep- adequate
Bowel and bladder movements- regular
Addictions- alcoholic for 7 years
Smoker for 4 years
Tobacco chewing since 5 yrs
Family history-
Not significant
He came here on
10/2/22
with cc of pus discharge from left upper molar since 2 months.
General physical examination-
Patient is conscious coherent cooperative well oriented to time place and person.
We'll built and nourished.
Pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema - absent
VITALS on admission
Temperature- afebrile
Blood pressure- 120/90
Resp rate-19cpm
Heart rate- 81bpm
Intra oral examination-
Extra oral examination-
Eye examination-
Direct light reflex +
Consensual light reflex+
Extra ocular movements on all sides+
Spheroidal degeneration over cornea
ECG-
Provisional diagnosis: Chronic suppurative osteomyelitis
D/D: Oro antral communication
11/02/22
Referred to Dept. of oral and maxillofacial surgery
OPG is done. ( reveals periapical radiolucency Lvl 26+27)
Provisional Diagnosis: Osteomyelitis of the left maxilla
12/02/22
ENT referral taken:
O/E : nasal mucosa congested.
Mild dns to right with rt ITH
Mild tenderness over left cheek.
Nasal endoscopy done :
First pass - dns to right
Second pass- N
Third pass: thick yellowish mucoid discharge in the middle meatus area (left)
Pus sent to culture and sensitivity
RBS, LFT suggested
Provisional Diagnosis: Lt oroantral fistula with chronic maxillary sinusitis
RBS - 154mg/dl
S. creatinine - 0.8
Blood urea - 12mg/dl N
Na+ - 132, K+ - 3.8, Cl- - 98
Serology -ve
CT PNS -
pus discharge from left 2nd upper molar tooth showing connection with temporal lobe
Rx: Inj. Cefotaxime 1gm IV/BD
Inj. Metrogyl 100ml
Inj. PAN 40mg IV/BD
2% Betadine gurgles dilute with water 2-3 times/ day
Tab. Acetelofenac + PCM
14/02/22
CECT Neck done
Provisional diagnosis: Lt oroantral fistula with chronic maxillary sinusitis, Lt spheroid degeneration
Rx: Inj. Cefotaxime 1gm IV/BD
Inj. Metrogyl 100ml
Inj. PAN 40mg IV/BD
2% Betadine gurgles dilute with water 2-3 times/ day
Tab. Acetelofenac + PCM
15/02/22
Pus sent for culture + sensitivity test
Enterococcus species grown. Sensitive to all the drugs.
Gram stain in favor of anaerobic infection
Most likely fusobacterium species
Rx: Inj. Metrogyl 100ml
Inj. PAN 40mg IV/BD
Inj. Augmentin 1-2g,m IV/BD for 5days
Inj. Voveran 75mg IM BD for 5 days
Chlorhexidine mouth wash TID
Treatment plan : enucleation and curettage under GA
16/02/22
CECT neck was done which revealed
Expansile unilocular lytic lesion involving the maxillary arch on the left side bulging in the lumen of the left maxillary sinus
F/S/O Locally aggressive odontogenic/non-odontogenic lesion of the jaw
Suggested HPE correlation
The lesion is causing significant narrowing of the maxillary sinus and reaching up to the orbital floor superiorly.
Other extensions as above
Cervical lymphadenopathy as above
Incision and drainage was done.
Biopsy sample sent
HbA1C - 6.8
GRBS - 72mg/dl (8 am), 74mg/dl (2 pm), 140mg/dl (8 pm)
19/02/22
relatively little pus oozed out since today morning
no more oozing of blood from the site of the biopsy incision today. Last happened yesterday morning
BP - 100/80mmHg, PR - 76bpm, RR - 20cpm, GRBS - 120mg/dl
Pus collected:
20/02/22
relatively little pus oozed out since today morning
no more oozing of blood from the site of the biopsy incision today.
21/02/22
relatively little pus oozed out since today morning
BP - 110/80mmHg, PR - 72bpm, RR - 18cpm, GRBS - 103mg/dl(8 am), 250mg/dl(2 pm), 84mg/dl (8 pm)
22/02/22
relatively little pus oozed out since today morning
BP - 110/80mmHg, PR - 80bpm, RR - 18cpm, GRBS - 104mg/dl
Provisional Diagnosis: Osteomyelitis
Histopathological findings:
H & E stained section show the presence of parakeratinised stratified sq. epithelium of variable thickness along with underlying connective tissue stroma. The epithelium does not show any dysplastic features. The underlying connective tissue stroma is composed of dense collagen fiber bundles and chronic inflammatory cell infiltrate chiefly composed of lymphocytes. Hemorrhagic areas are also seen in the given specimen.
The above histopathological features suggestive of inflammatory lesion
Provisional diagnosis-
Infected odontogenic cyst of left maxilla with osteomyelitis; Lt oroantral fistula with chronic maxillary sinusitis, Lt spheroid degeneration with Denovo DM type II
Rx: Inj. Augmentin 1.2gm IV/BD
Inj. Gentamycin 40mg in 100ml NS over 30mins TID
Inj. voveran 75mg IM/BD
Inj. PAN 40mg IV/OD
Chlorhexidine mouth wash TID
27/02/22
Scanty pus discharge into the mouth
Pain completely releived
Pus collected:
Treatment:






















Comments
Post a Comment